Many scleral lens practitioners experience frustration with a time-consuming scleral lens fitting that seems to go nowhere. Commonly described as “chasing (our) tails,” an issue with the lens fit or over-refraction seems to be unresolvable despite multiple changes that may even intensify the problem. Discussions with your consultant can be pivotal to the success of the scleral lens fitting and may even help retain patients at your office for future refittings.
So, what should be communicated with the consultant?
Exam Notes:
Detailed notes can provide consultation with important information including:
Lens ID and Wearing Time: Visionary Optics’ lenses are all engraved with a unique Lens ID infero-temporally. You can find more information regarding lens markings here.
Lens Rotation: The hashmarks on a diagnostic lens delineate the Steep meridian of the landing zone.
- The hashmarks on the patient’s lens should align at 3 and 9 o’clock regardless of landing zone toricity.
- The location of markings can be notated in clock hours or in degrees, and rotation should be noted as either clockwise (CW) or counterclockwise (CCW) for clarity.
- If possible, try to notate the rotation in degrees by rotating the slit lamp beam to align the hashmarks. This provides more accuracy especially if front surface optical toricity is needed.
Over-Refraction
As with any contact lens, performing an over-refraction is crucial for patient success.
- If the power is over -/+ 4 diopters, it will need to be vertexed. Good news! You do not need to do the vertexing, but if you do, please inform the consultant.
- If the lens is multifocal, check near and distance acuities and provide that information to the consultant. Stay tuned for optimizing multifocals in a future edition of our newsletter!
Lens Centration
- A scleral lens often decenters infero-temporally to some degree; decentration can be measured by comparing the distance between the limbus and the edge of the landing in all 4 quadrants.
Corneal Clearance
- With diagnostic lenses, clearances can be measured at the slit-lamp using white light or cobalt filter with fluorescein (NaFl) in the bowl of the lens.
- The clearance under the lens should always be compared to the lens thickness as this is a consistent value that will be provided with the list of lens parameters. Typically, a 1:1 ratio on insertion is desired. Diagnostic lenses have a center thickness of 400 µm and patient lenses typically have a center thickness of 300 µm. If there is a high plus power the center thickness may vary, so please check the parameters listed on the packing slip.
- Always remember that scleral lenses can settle as little as 50 µm to 175 µm or more with time. That is why it is always crucial to document wearing time.
- Caution: If you remove the lens after it is settled and reapply it with fluorescein, you have lost your settling of the clearance. Try to get in the habit of determining clearances without NaFl.
- In keratoconus, central clearance is important, but what is more important is clearance over the apex of the cone. Make sure that there is adequate clearance over the cone, and sometimes that may result in high levels of central clearance which may be unavoidable.
Landing Zone/Haptic
- Areas where the landing is not ideal should be noted in clock hours or degrees, and the severity of the issue should be graded or more concisely defined.
- Compression: This is where the conjunctival vessels are blanched, and the conjunctiva looks more “white” compared to the rest of the tissue. This is related to the lens pushing down on the tissue and being too tight in that area. It can be at the edge of the landing zone, or in the middle. This will cause rebound hyperemia in that area when the lens is removed.
- Impingement: This is where the edge is digging or pinching into the conjunctival tissue. It may be hard to see when the lens is on the eye, but it will always cause conjunctival arcuate staining after the lens is removed.
- Edge lift: When a patient is symptomatic immediately after lens application, it is often related to edge lift. It will be easily identified with NaFl at the edge. Shadows at the edge are often seen where lifting is present.
Lens Surface Quality/Wettability
- In instances of poor wettability, checking with the patient on their care and handling regimen can give insight into whether the issue is relating to the lens material and coating selection or if external factors are the cause.
- Lenses can also be scratched, and the patient may be removing the lenses from the cases harshly. Patient education is important and handling practices should be reviewed on follow up visits.
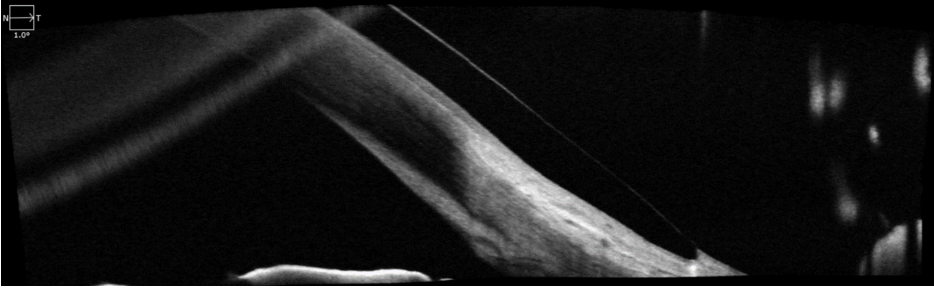
Optical Coherence Tomography (OCT)
In more recent years, OCT has become a popular tool for eyecare providers in the scleral lens fitting process due to its ability to precisely measure clearances and display the relationship of the lens to the eye surface. OCT is not required to fit a scleral lens but will usually aid in the fitting process and may result in fewer overall visits when optimizing the overall fit.
Figure 1. Anterior OCT showing the temporal landing of a Europa Tangent scleral lens. (Image courtesy of Kendall Shafran, OD)
If choosing to use OCT, it is preferred that imaging be taken in the following areas:
- Centrally over the cornea to determine clearance
- Over the apex of the ectasia in irregular cornea patients
- Peripherally over the limbus
- Along the edge of the haptic in all 4 quadrants
- Any problem areas including areas of edge lift/bearing, corneal touch, limbal bearing, etc.
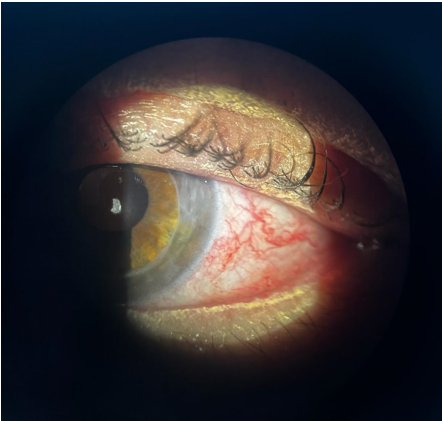
Slit-Lamp Photography
With the popularity of smartphones, it is easier now more than ever before to capture the images of lenses on the eyes while the patient is in the exam chair. Although photos can be taken by simply holding the phone camera near the ocular, several products exist on the market that allow the user to mount the phone to the exam station or to the slit-lamp directly.
Slit-lamp photography can be used to give a visual of areas with needed improvement such as surface wettability, blanching/impingement, areas of corneal touch (when NaFl has been applied), edge lift and other fitting concerns. Photos like these become particularly useful when a quadrant-specific modification such as a precision-lift or notch needs to be applied to the lens haptic. Also, images of the eye after lens removal are equally useful to demonstrate corneal or limbal staining, rebound hyperemia, conjunctival staining or other anomalies.
Figure 2. Slit-lamp photography showing rebound redness and conjunctival inflammation post lens-removal. (Image courtesy of Nathan Schramm, OD, FSLS at Insight Vision Center Optometry, CA)
Photos can also be taken by the patient at home if they are reporting issues that occur outside of the office. For example: redness on removal, general discomfort, and dryness can be given more context from a single photo.
The Takeaway
Documentation and imaging will always be a useful tool between you and your consultant when optimizing patient fits. This may result in enhanced patient comfort and reduced chair time before finalizing a design. These suggestions are useful for problem fits; however clear documentation and image acquisition are always useful in scleral lens management. These steps by provide a reference for future visits and develop a thorough routine with all of your scleral lens fits.
At the end of the day, don’t hesitate to reach out to Consultation! Our team is here to help you with all your scleral lens fits with Visionary Optics at all levels of complexity.