During examination, patients might complain of clouding, fogginess or blurry vision which oftentimes can be attributed to midday fogging (MDF). Depending on the frequency and severity of symptoms, several causes can contribute to this pathology.
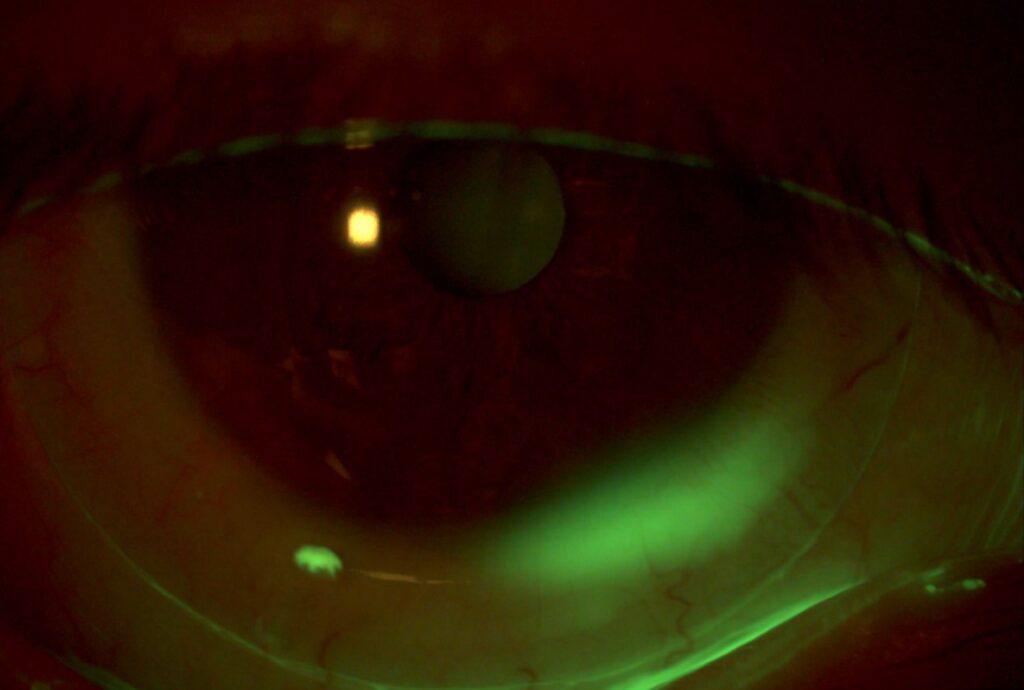
Fine, white diffuse particles in the fluid reservoir
- Possible source: sloughed corneal epithelial cells due to an inflammatory response (1)
- Resolution:
- Utilize an ionic filling solution
- Apply preservative-free viscous lubricating drops to the fluid reservoir
- Decrease central clearance
- If impinging/digging at the edge: Flatten haptic in the absence of tear exchange
- Apply a toric haptic or quadrant-specific modification in the presence of tear exchange by aligning and tightening the area of excessive tear exchange
- Talk with consultation!
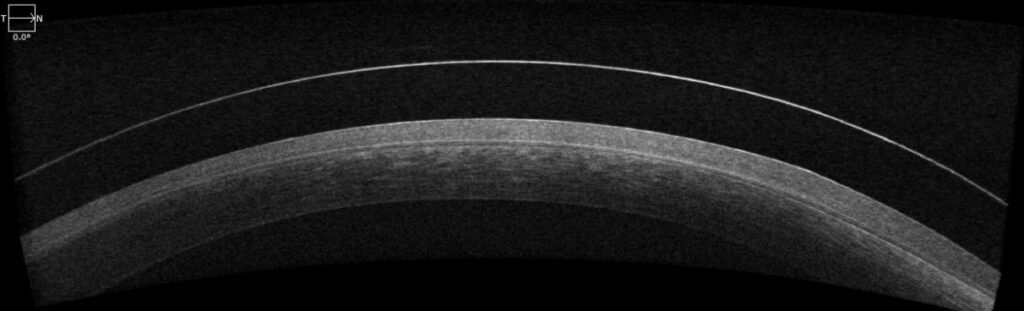
Figure 1. Fine particulate matter within the fluid reservoir. (Image courtesy of Renée Hanson, OD)
Yellow or brown droplets in the fluid reservoir
- Possible source: excessive meibum or lipids (2,3)
- Resolution:
- Assess lids and lashes for MGD or blepharitis and treat with the appropriate measures
- Decrease central clearance
- Apply preservative-free viscous lubricating drops to the fluid reservoir
- Apply a toric haptic or quadrant-specific modification in the presence of tear exchange by aligning and tightening the area of excessive tear exchange
- Talk with consultation!
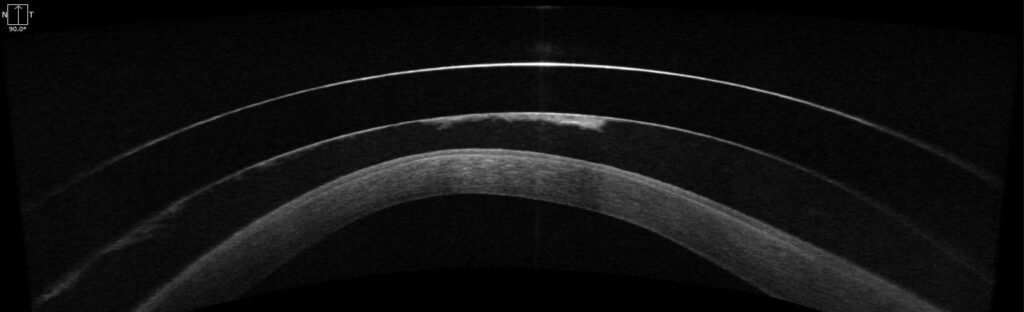
Figure 2. NaFl uptake under the infero-nasal quadrant. (Image courtesy of Krista Mathson, OD)
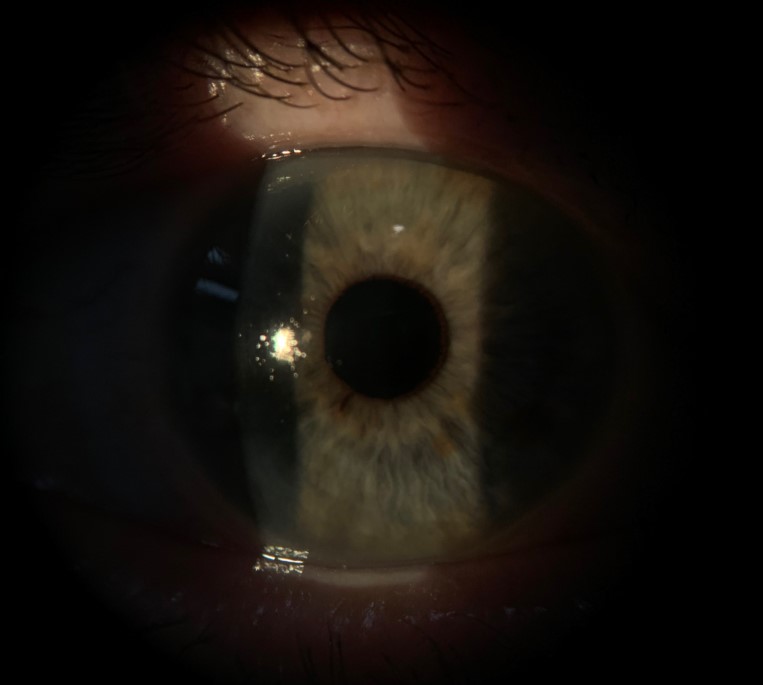
White globules in the fluid reservoir
- Possible source: mucin, most often from the presence of excessive tear exchange or giant papillary conjunctivitis (3)
- Resolution:
- Decrease the central clearance
- Treat giant papillary conjunctivitis if present
- Apply a toric haptic or quadrant-specific modification to more closely contour the scleral shape without impingement or compression
- Apply preservative-free viscous lubricating drops to the fluid reservoir
- Talk with consultation!
Figure 3. Large globule-like infiltrates underneath a scleral lens with no other visible particulates. (Image courtesy of Connie Chen, OD, FAAO)
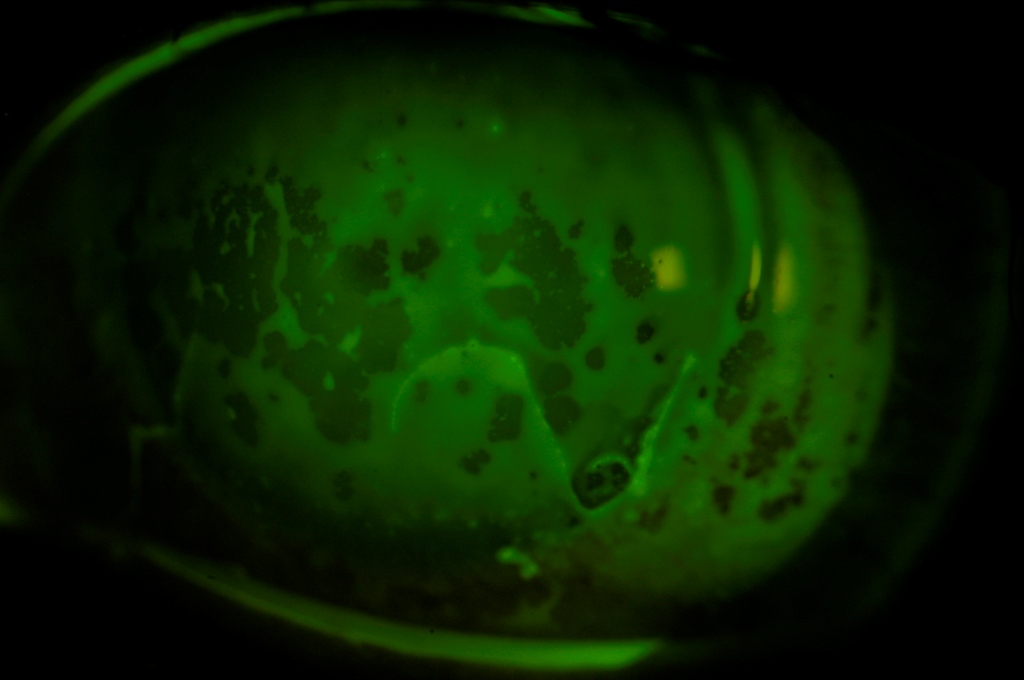
White buildup or oily deposits on the front-surface, or poor wettability
- Possible source: excessive lipids (MGD, ocular rosacea, graft-versus-host-disease, Stevens-Johnson syndrome, Sjögren’s syndrome, etc.), inadequate lens hygiene, the use of oil-based products-makeup, lotions, moisturizing hand soaps etc. (3)
- Resolution:
- Assess lids and lashes and treat with the appropriate measures
- Change the lens material to a lower Dk and lower wetting angle
- Apply Hydra-PEG® coating but be sure to use compatible solutions with Hydra-PEG®
- Modify the patient’s lens care regimen to limit possible exposure to any oil-based products during application and removal (A&R)
- Switch to a peroxide-based system for lens cleaning and storage if patient has sensitivities
- Introduce a stronger chemical cleaner for biweekly maintenance (i.e. Progent)
- Talk with consultation!
Figure 4. Oily deposits over the front surface, visible with white-light. (Image courtesy of Jenny Wong, OD)
Figure 5. Non-wetting lens, visible with NaFl behind a cobalt blue filter. (Image courtesy of Lynette Johns, OD, Visionary Optics Director of Clinical and Scientific Affairs)
Unresolved MDF
In cases where patients do not experience resolved symptoms or see minimal improvement, lenses can be re-applied midday with fresh solution to flush out debris that has built up within the FR. Patients should also keep a scleral lens kit on hand which includes all the necessary tools for proper A&R and maintain excellent hygiene during lens handling for optimal results. In dirty or dusty environments, there is also the option of utilizing protective eyewear to minimize lens exposure to external debris.
Final thoughts
When a patient experiences MDF with their scleral lenses, take the time during an exam to evaluate the frequency of the symptoms and possible causes. Narrowing down possible causes using lissamine green or sodium fluorescein in addition to reviewing patient care and handling can greatly reduce overall chair time and the number of visits required, in addition to keeping your patients happy with their lenses. If OCT is available, capturing imaging of the central clearance in addition to all 4 quadrants of the haptic will also aid in determining possible modifications needed to reduce resolve MDF. Our consultation team is always here to help you address the challenging problem.
- Postnikoff CK, Pucker AD, Laurent J, Huisingh C, McGwin G, Nichols JJ. Identification of Leukocytes Associated With Midday Fogging in the Post-Lens Tear Film of Scleral Contact Lens Wearers. Invest Ophthalmol Vis Sci. 2019 Jan 2;60(1):226-233. doi: 10.1167/iovs.18-24664. PMID: 30646011; PMCID: PMC6340400.
- Walker MK, Bailey LS, Basso KB, Redfern RR. Nonpolar Lipids Contribute to Midday Fogging During Scleral Lens Wear. Invest Ophthalmol Vis Sci. 2023 Jan 3;64(1):7. doi: 10.1167/iovs.64.1.7. PMID: 36630141; PMCID: PMC9840443.
- Carrasquillo, KG, Lipson MJ, Ezekiel DJ, et al. Chapter 12 Scleral Lens Complications and Problem Solving in Barnett M, Johns LK. Contemporary scleral lenses: theory and application. United Arab Emirates: Bentham Science Publishers, 2017:395-404